更多
分享

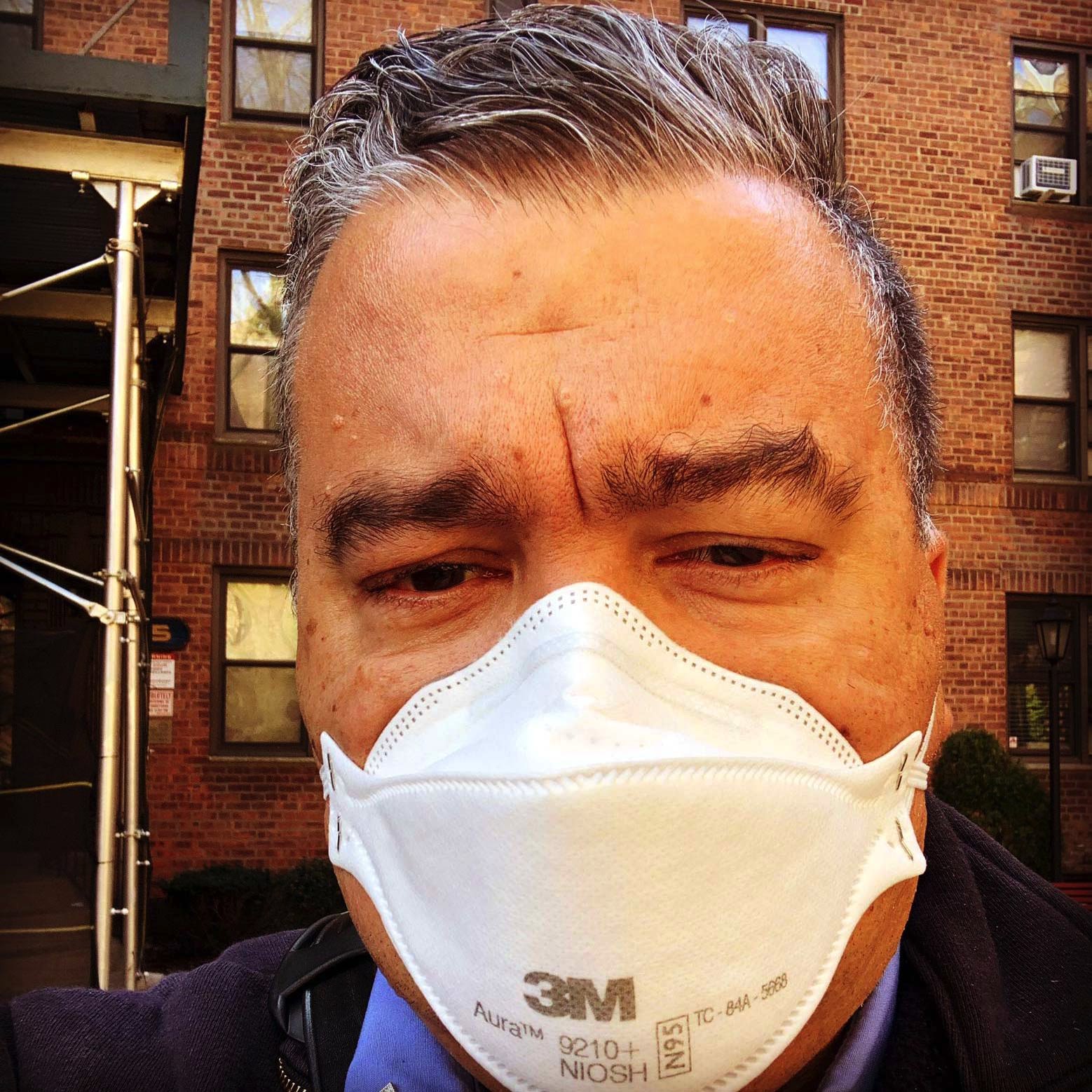
安東尼·阿爾莫傑拉(Anthony Almojera)是美國紐約的一名資深急救員。他是紐約消防大隊醫療急救隊副隊長,也是紐約緊急醫療服務人員工會消防支部副主任。在他17年的緊急救護生涯中,見證了無數生死險情,可謂見過"大世面"。但這一切都不足以讓他為新冠疫情大爆發做好心理凖備。
美國已經成為全球疫情最嚴重的國家,無論是死亡人數還是確診病例都高居榜首,而紐約則是美國的疫情中心。
作為救護人員,安東尼每天戰鬥在疫情的最前沿,爭分奪秒挽救人們的生命。同時,他還要與團隊成員緊密合作、相互支持,因為他們也在為自己和家人的生命擔憂。
安東尼在接受BBC記者愛麗絲·庫迪(Alice Cuddy)採訪時,講述了他4月5日當值那天24小時的經歷。他說,這是他職業生涯中最艱難的一天。
以下是他的口訴:

儘管前一天各種求救電話和緊急情況讓人忙得不可開交,但我昨晚睡得很香,一連睡了整整5個小時。早晨起牀後,邊淋浴邊聽新聞。新冠病例繼續攀升,但世界似乎仍在完好運轉。
我必需要在早晨六點鐘趕到工作地點,位於布魯克林的日落公園,開始一天16個小時的救護工作。
我穿好制服,拿上我的無線對講機,開始給我所有的設備消毒。
我們每天必需要給所有的無線通訊設備、鑰匙、車、袋子等等徹底消毒。因為這個病毒可以在任何地方存活,沒有什麼地方是安全的,包括跟你一道工作的同事們。
在戰爭年代,你面對的是子彈。你知道誰是你的敵人。然而,我們目前面臨的是一場無形子彈的戰爭,你所接觸的每一個人都可能是那枚讓你致命的子彈。

早晨6:02,我打開電腦開始登陸。我在百吉餅店(也叫貝果店,bagel shop)買了份早餐。大約7點左右,線路開始繁忙起來。
自從昨天午夜開始,我們已經接到了1500多個求救電話。我收到一個心臟驟停的求救電話。
作為急救隊副隊長,我會跟醫務人員和緊急醫療技術員一道去救治病人,並根據需要提供資源支持。但最近資源很有限,因為我們幾乎每天都會接到6500多個求救電話。
紐約市的緊急醫療服務(EMS)系統堪稱是世界上最繁忙的,平均每天接到大約4000個求助電話。但如果遇到熱浪或颶風這樣的緊急情況,求助熱線電話數量會飆升。
但在新冠疫情之前,最忙的一天要數9.11恐襲那一天。那天,我們接到了6400個電話,但那並不是6400個病人。許多人當時被困在世貿大樓中,要麼能逃出來生還,要麼喪生。
現在每天的求助人數超過了9.11,而且都是實實在在的病人。
我們注意到大約在3月20日左右,病例開始激增,到22日簡直要爆了。問題是我們的系統跟不上,我們的資源也有限,真不知如何能應對。但我們還是全力以赴。
目前,我們大約有20%的緊急醫療服務人員在生病,我們也有許多工作人員感染了新冠病毒,甚至有人進了重症監護病房,其中兩人需要使用呼吸機,病情十分嚴重。此外,還有700多人出現新冠症狀,正在自我隔離和密切觀察中。
一天,我們來到一戶人家。我穿戴好防護服、口罩和手套。我們看到一名男子,他家人說他發燒、咳嗽已經5天了。我們開始為他實施心肺復蘇術。為了幫助他呼吸,醫務人員為他插了管,並開始給他靜脈注射。
我們一共搶救了半個小時,最後還是沒能把他救活。事後,我要保證我的團隊平安無事,然後回到車裏再次進行消毒。一切進行完畢後,我按下按鈕,凖備接下一個任務。
20分鐘後,我們又接到了一個心臟驟停的求助。我們出發抵達出事地點。不幸的是,同樣的症狀、同樣的步驟、同樣的結果。
新冠主要攻擊病人的肺部,讓人缺氧。隨著病情加重,身體其它器官開始衰竭和關閉,最終導致死亡。
接下來的求助電話幾乎都是跟新冠有關的,只有一個是因為自殺。你可以想象,當我接到自殺電話後的那種如釋重負的感覺。雖然,這個人因為自殺身亡,但它至少不是因為新冠而死的。
到上午11點時,我已經處理了6起跟新冠有關的心臟驟停病例。在正常情況下,我們大概每周會有兩、三起心臟驟停病例。
雖然,有時我們也會非常忙,但絶不會像現在這樣。不可能像現在這樣。
對我打擊最大的是我當天接到的第7個電話。
當我們到那裏時,看到一位女士為躺在地上的母親做心肺復蘇術。她告訴我們她母親出現新冠症狀,然後呼吸暫停。
在我們的急救護人員設法搶救她母親之際,我走過去向這個女兒了解情況。她告訴我母親已經病了幾天。他們無法做新冠測試,但覺得肯定是感染了病毒。
我問她,她是否是唯一的親人? 她說是的。但她接著告訴我,我們救護隊前幾天剛來過,當時搶救的是她父親,但也沒能救活他;他也有新冠症狀。她說這話時臉上表情麻木。
我走到醫護人員搶救她媽媽的房間,希望他們能告訴我她媽媽還有生命跡象。但是,當我看到醫生的眼神時我就知道她媽媽已經不行了。
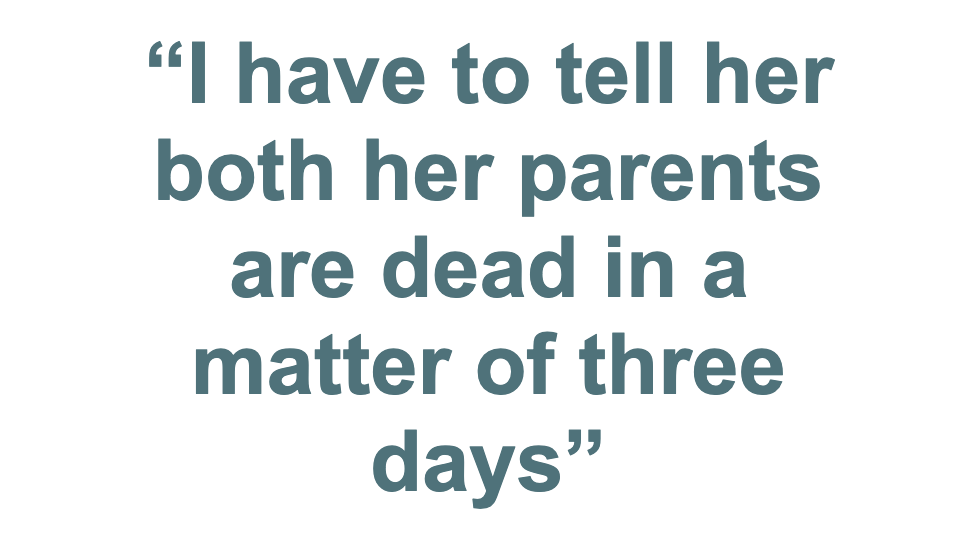
從我從事這個職業17年的經驗,通過眼神我就能夠判斷答案。而我現在不得不把這個壞消息告訴這位女兒。她的父母在三天之內雙雙撒手人寰。
她父親當時甚至還沒有下葬。所以,這意味著她將會給爸爸媽媽同時舉辦葬禮。但這得看她的運氣如何,因為在當前情況下很難正常辦喪事。
接完這單任務後,我走到屋外;我需要冷空氣清醒一下。
我們靜靜地坐了一分鐘,設法讓心情平靜一下。雖然沒有人說話,但大家都心有切切。遇到這種事,救護人員往往會沉默無語,不討論。

我們必須繼續工作。我們又開始接下一個任務。就這樣,我們處理了另外幾個求助電話。
大約在晚上6點左右,我剛完成當天的第10個救護任務。下一個呼救的是一個亞裔家庭。他們的叔叔剛剛過世,但他們無法相信這是真的,從他們的眼神中我可以看得出來。
他們就是不相信他已經死了,不斷地懇求我救救他,讓我把人送到醫院去。我告訴他們這樣做無濟於事,因為人已經沒有任何生命跡象,送去醫院也沒用。
但他們仍然一再懇求我,讓我們一定要救活他。期間,死者的兒子問我們為什麼不能恢復他的心跳,我們真的是無言以對。
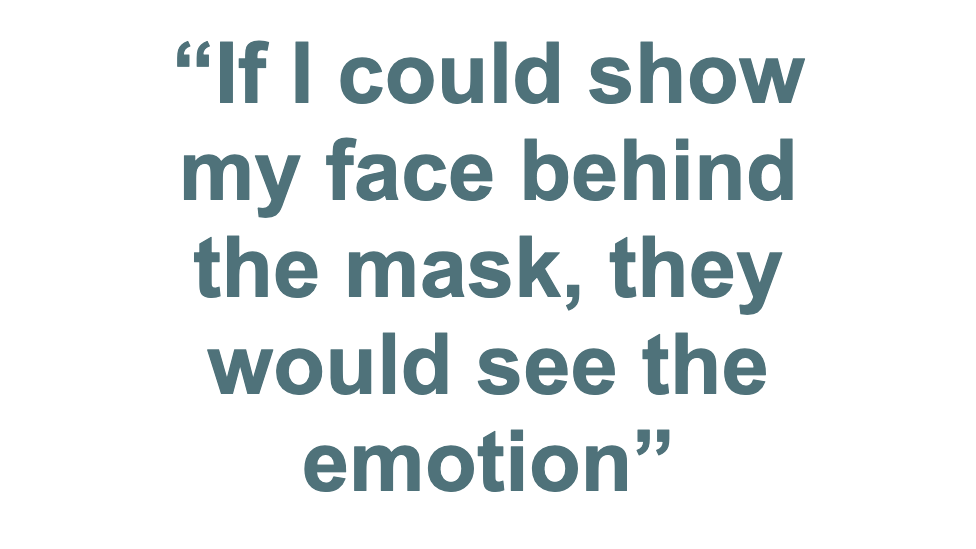
最難的是因為我們都帶著口罩,所以,他們只是聽到了我們的話,無法看見我們的表情。如果我能摘下口罩,讓家屬看到我的表情,他們就會明白。
但他們只看到我的眼睛,我的眼中充滿了恐懼,因為我不知道如何才能使這位兒子相信,我們真的是無能為力,回天無術了。

那個失去雙親的女孩給我的打擊最大。在我的職業生涯中,從未遇到過像這樣的一天,令我惶惑,難以自製。
我不得不向10個家庭解釋,我們無法救活他們的親人,我們無能為力了。
這種事情有時很難讓人忘懷。經歷這些事情肯定會對人有影響。我敢說大多數緊急醫療服務人員都會受到影響,不可能再像以往那樣輕鬆自在了。
也許,有些人可能看得透徹,能夠欣賞生活中美好的事情,比如,鮮花和日出。但對我們大多數人來說,一閉上眼睛就會看見這些場景,揮之不去。
兩位醫護人員看到我做在外面,他們走到我身邊坐下,然後伸出手臂抱住我。在這至暗時刻我們相互支持和安慰。
我們無需語言,都知道彼此此刻的感受。我們休息了片刻,就又開始接手下一個任務。

到了晚上9點半,離我下班間還剩半個小時,我們又接到一個心臟驟停電話,還是同樣症狀:發燒、咳嗽了幾天后就不行了。
我們同樣進行急救,同樣沒有回天之術。我不得不通知家屬這個不幸的消息。這已經是我這天班上第12次告訴病人家屬同樣的消息。我從未這樣疲憊過,心力交瘁。
我是單身漢,沒有孩子。這是我這輩子唯一對此感到欣慰的時候,因為我不必擔心會把病毒帶回家。許多同事都非常擔心自己會傳染給家人。
我的工作性質意味著我有可能會在工作中生病和死亡。而那些有家屬的同事,他們的家人知道他們的親人有可能會因公殉職,但未必知道他們的親人還有可能把病毒帶回家。
我的一些同事乾脆在車裏過夜,就是不想把病毒帶回家,感染他們的親人。
我的同事們擔心的是萬一他們因公殉職家裏沒人照顧。這對我是巨大的壓力。

我自己接受心理治療有16年了。我還信佛教,經常打坐。但即使這樣,我現在都難以排遣這種衝擊。
這種經歷對人的情感折磨日復一日的跟隨著你,因為你知道明天你還要面對16個小時的救護工作,你還會碰到同樣的場景和問題,無處逃遁。
作為醫療救護人員,我們知道無法救活每一個人。但是,我們總是寄希望於救活下一個患者,這樣才能讓你感覺好一點,才能把工作繼續做下去。我們通常是善於挽救生命的。
然而,從目前來看這一病毒正在減少我們勝算的機會,讓我們看不到希望。我們正在跟新冠病毒這個隱形的敵人作戰。為此,我們許多同事失去了寶貴的生命。
希望正在一點點消失,全紐約都在發生同樣的事情。
注:在安東尼這天班上死亡的12名疑似病例沒有一人接受過新冠病毒檢測。因此不會計入紐約官方新冠死亡數據中。
紐約市這一天(4月5日)的死亡人數為594例。
I got a pretty good night's sleep considering all the calls going on the day before. A solid five hours. I get up and listen to the news in the shower. More Covid-19 but the world still seems intact. I have to get ready to be at work in Sunset Park, Brooklyn, at 06:00 for a 16-hour shift.
I put on my uniform, grab my radio and start the process of decontaminating my equipment. We have to wipe down all the radios, keys, trucks, bags and the rest of the gear. This virus can stay alive on everything. Nothing is safe - even your co-workers.
In wars you see the bullet, you know who your enemy is. This is a war with an invisible bullet - everyone you come into contact with is a bullet who could get you.
I log on that morning at 06:02. I'm able to go get a bite to eat at the bagel shop. I start to hear the radio get busy around 07:00. We have already had more than 1,500 calls since midnight. I get called for the assignment - a cardiac arrest.
As a lieutenant I go with the medic and emergency medical technician crews to help treat patients and provide resources as needed. These days there aren't many resources as most days there are well over 6,500 calls.
New York City has the busiest emergency medical services (EMS) system in the world - with about 4,000 calls a day on average. Sometimes you get a spike like with a heatwave or a hurricane, but the busiest day before this was 9/11. That day, we had 6,400 calls but that wasn't 6,400 patients - either you made it out or you didn't. This is 9/11 call volume with patients every day.
We noticed the spike in cases around March 20. By the 22nd it was like a bomb.
When we saw this spike, the system wasn't set up for it. We were like: 'How are we going to do this with the resources we have?' It was just a case of 'let's get going'.
Right now, about 20% of the EMS workforce is out sick. We have a lot of members who've contracted Covid-19, we have members who are in the ICU - I have two of them who are on ventilators - and we have over 700 people who are being monitored with the symptoms.

We arrive at the house and I put on my mask, gown and gloves.
We find a man. His family says he has had a fever and cough for five days. We start CPR and I watch the medics pass a tube down his throat to breathe for him and the IV gets started.
We work on him for about 30 minutes before we pronounce him dead. I make sure the crews are OK and get back in my truck - decontaminating everything first. I hit the button to go available.
Twenty minutes later, I get another cardiac arrest. Same symptoms, same procedures, same results. This virus attacks the lungs: you can't get enough oxygen into your system, then other systems start to shut down and then organ failure.
We hit the button, get another one.
Hit the button after that, get another one.
There's only one patient we've seen so far who I feel wasn't Covid-19 and that's because it was a suicide. Imagine: I was there and my brain felt relief. This person's dead and it's a suicide. I felt relief that it was a regular job.
It is now around 11:00 and I've done about six cardiac arrests.
In normal times, a medic gets two or three in a week, maybe. You can have a busy day sometimes, but never this. Never this.

The seventh call gets to me.
We walk in and there's a woman on the floor. I see this woman doing CPR on her mother. She tells me she stopped breathing and had "the symptoms".
We go to work to try and save her. As the medics are doing their thing I walk over to the daughter and she tells me how it all went down. She says her mum has been sick for the last few days. They couldn't get a test but think she had "it".
I ask "are you the only family here?" She says yes but you guys were here on Thursday and worked on my dad. He had the symptoms as well. He passed away.
She looks numb.
I go back into the other room and hope that the medic will tell me there are signs of life. She looks up and I know the look after 17 years. The medic's eyes say no.
So now I have to tell the daughter that both her parents are dead in a matter of three days.
Her dad's not even buried yet. So this woman is going to have a double funeral, if she's lucky enough to get a funeral, because funerals aren't happening right now.
After that call I go outside and the cool air is what I need. We sit for a minute to try and recoup but we all feel it. Funny, we don't discuss it much. Medics tend to do that.
We have to get ready for the next one. We hit the button.

We get another one and so on and so on. It's about 18:00 and I just finished my tenth one.
It's an Asian family who cannot believe their uncle has died. I see in their eyes they can't believe it. They keep imploring me to do something, to take him to the hospital, and I tell them we couldn't, even if we wanted to. The hospitals are not working on anyone who has no signs of life.
They keep saying "you have to save him, you have to save him". The son asks why we can't just start his heart again.
The hard thing about wearing the mask is it covers half my face. All he's hearing are the words. If I'm able to show my face it lets the patient's family see the emotion behind it.
Now all they see is my eyes and my eyes are in terror because I don't know if I can convince this kid that there's nothing more we can do.

I'm on this call with the medics who were with me at the house with the daughter who lost both parents. They come outside and see me sitting on the stoop.
I've had to tell 10 families we couldn't do any more.
I am beside myself with feelings of bewilderment. I've never had to do a day like this in my career. I'm emotionally drained.
The things we see are sometimes difficult to shake. And with this, people are going to be different afterwards. There's no way that the majority of EMS workers are going to come out of this happy-go-lucky. Maybe some of them will have these moments of clarity and appreciate the flowers and the sunrise, but for a lot of us, when we close our eyes, we're going to see this.
The medics see me and come over and sit next to me. They both put their arms around me and we support each other.
It was their fifth arrest that day. All of us know what we are feeling. We just feel it together for a bit. We sit and then hit the button.

It's 21:30 - half an hour to the end of my tour. Another arrest. Same symptoms - fever and cough for days.
We work on him until I have to go and tell my twelfth family that I'm sorry we can't do any more. I've never been so drained and I go back to get ready to go home.
I'm single and have no kids. This is the only time in my life that I've ever been happy that I'm single because I don't bring it home. But so many people are worried about this.
I signed up for a job where I can get sick and die. Members' families signed up knowing that their loved one could get sick and die on this job, but they did not sign up for the loved one to bring it home to them. Right now I have guys who sleep in their car because they do not want to bring it home to their families.
The stress that members have that weighs heavily on me is their worry that if they die on the job their families won't be taken care of.
I'm 16 years in therapy, I'm a practising Buddhist and I meditate, but even I'm having trouble disconnecting now. The emotional drain that happens on days like this stays with you because you know you're going to have to go to work tomorrow for another 16 hours and you're going to get it again.
Medics survive a career in this because we always have hope that OK, we didn't save this one but the next one we will save. We are pretty good at saving people's lives. But with this virus the odds are against us. Hope fades fighting it. We are fighting an invisible enemy that is taking out our co-workers - and right now, hope is fleeting.
This is happening all over the city.

Not one of the 12 people suspected to have died of Covid-19 on Anthony's shift had been tested for coronavirus. As a result, their deaths were not included in the official coronavirus death toll in New York last Sunday, which stood at 594.